I used to do pretty well in school, but I failed my sleep test.
I recently spent the night at a Sleep Center to participate in a sleep study to see if I have obstructive sleep apnea.
Find a Sleep Center near you.
The following information might help you if have sleep problems of any kind and you plan to participate in a sleep study test (or polysomnogram) in the future.
Reasons For A Sleep Study
My doctor (a general physician) has wanted me to have a sleep test for about a year.
I have not been feeling well-rested after a full night’s sleep for about that long.
After discussing other possible culprits (caffeine intake, medicines, exercise, sleep habits, relaxation before sleep, etc), she recommended the sleep study.
By the way, here are some of the signs & symptoms of sleep apnea:
- Snoring
- Daytime sleepiness or fatigue
- Restlessness during sleep
- Sudden awakenings with a sensation of gasping or choking
- Dry mouth or sore throat upon awakening
- Intellectual impairment, such as trouble concentrating, forgetfulness, or irritability
- Night sweats
- Sexual dysfunction
- Headaches
The pattern of snoring is associated with episodes of silence that may last from 10 seconds to as long as a minute or more. The end of an apnoea episode is often associated with loud snores, gasps, moans, and mumblings. Not everyone who snores has apnoea, by any means, and not everyone with apnoea necessarily snores (though most do). This is probably the best and most obvious indicator. Source
Sleep apnea is a chronic health condition that shouldn’t be taken lightly. Sleep apnea episodes (especially those associated with obstructive sleep apnea) can lead to serious heart issues, among other things.
OSA is a potentially life-threatening condition. Someone who has undiagnosed severe obstructive sleep apnea is likely to have a heart attack, a stroke, cardiac arrest during sleep, or a harmful accident. Source
My Sleep Test Room: First Impressions
I arrived at the Sleep Center at 7:30 PM.
I was told to bring pajamas, my own pillow, any medications, snacks I might want, and toiletry items for an overnight stay.
The private room I was given had:
- a double bed
- television
- DVD player (you can bring your own movies)
- private restroom
- the most comfortable recliner I have ever sat in – it was huge and leather.
- a monitoring camera next to the TV
- an audio monitor next to the bed
I met Sandy, my sleep tech. She asked me what time I wanted to go to sleep. I didn’t really know what to say — so I said my normal time: 11:00 PM.
 Sandy was very clear to mention that the camera and audio monitoring would not be turned on until I was to begin sleeping, as they respected my privacy. I did wonder how I could be sure about that, so I restricted my dancing and singing to a minimum .
Sandy was very clear to mention that the camera and audio monitoring would not be turned on until I was to begin sleeping, as they respected my privacy. I did wonder how I could be sure about that, so I restricted my dancing and singing to a minimum .
She gave me some paperwork to fill out. The paperwork asked all kinds of questions about my sleep patterns and how tired I was during the day. After filling out the required paperwork, I was on my own to hang out until it was time to hook me up for the sleep test.
I watched TV and read a magazine — wondering why I was there so early. I guess they want you to have some quiet time and relax before the sleep test starts.
The Sleep Center I was in can have as many as 6 patients each night, with 3 sleep techs each assigned to 2 patients. On my night there were only 5, because 1 sleep tech had a 6-year-old child — and parents are required to stay/sleep in the same room until kids are 16.
Getting Fitted For CPAP Masks
While I was relaxing, Sandy came in to fit me for potential CPAP masks (Continuous Positive Airway Pressure).
If I did demonstrate sleep apnea, then I would have to wear a CPAP mask for the second half of the night — experimenting with different airflow to see if it helped with the apnea.
 First, my sleep tech Sandy asked me if I breathed through my nose or my mouth. Unless I have a cold, I tend to breathe mostly through my nose.
First, my sleep tech Sandy asked me if I breathed through my nose or my mouth. Unless I have a cold, I tend to breathe mostly through my nose.
She showed me 2 different kinds of masks:
Sandy started with the nasal CPAP mask and fit it over my nose — adjusting the straps around the top of my head and my face (forehead and under my mouth) to the back of my head. The mask reminded me of an oxygen mask, and it was very, very tight. It was much closer to my eyes than I had expected — and honestly, it kind of freaked me out. Then she turned the air flow on, and this was also very strange. It felt like air was being forced in and out of the mask, like it was forcing me to breathe at that rate. This was my first moment of being uncomfortable, and I wished I had done more research on this ahead of time.
This video describes the air pressure very well:
And here is a good one showing how the CPAP works:
Next, Sandy tried the full face CPAP mask — this one fit tightly over my nose and mouth, and also felt very close to my eyes. She turned on a light pressure, and I tried to say, “Let’s take this off” – but I couldn’t talk at all! I felt a bit more freaked out and started to pantomime “off”. Sandy said, “Oh, are you having some anxiety?” Yes, Sandy, yes I am! Before this, I did not think of myself as claustrophobic at all — but now I think I know what claustrophobia might be like.
I didn’t ask any questions about how the CPAP was working, and Sandy didn’t offer any information.
If I had to do it all over again, I think I would try to be much more prepared for things like this CPAP mask experience.
Getting Hooked Up To The Sleep Test Sensors
At about 10:20 PM (Sandy was delayed with her other patient), it was time to begin attaching all the sensors that would take readings of — well, pretty much everything!
The first sensors (electrodes) that she put into place were:
- 2 on each calf muscle — to measure “crawling leg” or Restless Leg Syndrome
- 2 on my chest and 1 on my back — to measure heart rate
- Several snapped onto soft elastic straps across my chest and abdomen — to measure breathing movements
 These electrodes were all attached with sticky pads — covered over with medical tape. Each had a long, thin wire that plugged into a data box to transmit the data to a computer in the monitoring room, which was down the hall.
These electrodes were all attached with sticky pads — covered over with medical tape. Each had a long, thin wire that plugged into a data box to transmit the data to a computer in the monitoring room, which was down the hall.
Next, Sandy started measuring my head — so she would know where to place the next electrodes.
These small (smaller than a dime) metal discs were connected to a wire and attached to my scalp with a type of glue called Ten20 Conductive Paste. Yep, glue. The materials they gave me before the sleep study test said the glue would easily wash off the next morning. They did not say that I would leave with huge, wet glops of glue on my head. (That would have been nice to know!)
Sandy spent about 10 minutes with a small tape measure — marking certain spots on my head with a red wax pencil. Before attaching the head sensor, she used a cotton swab stick thing and an antiseptic gel to clean the spot. And by clean, I mean rub the skin raw and remove any poor hairs from that area. It felt like she might have been drawing blood, reinforced by the red spots I saw on the swab when she was done! Before I panicked, she mentioned that she had to rub a little harder on my head — because the red wax marks had to be removed, as they would prevent the glue from sticking. (Whew, it wasn’t blood!)
She used the electrode to scoop a large mess of glue and place it gently on my head. Then, she used a gauze pad full of the glue (which was a consistency of thick Vaseline — not a runny glue) to forcefully (painfully!) PUSH the electrode onto into my scalp. Several minutes were spent push… Push… PUSHING the glue and the disc — to make sure they stayed right in the place they needed to be. She left the gauze pad on, to keep the glue somewhat contained.
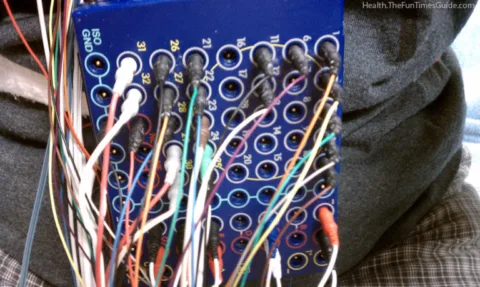
Each electrode was connected back to the same data box as all the others — seen here:
Next, it was time for the face sensors:
- 3 across my forehead — for additional brain measurement
- 1 at the corner of each eye — to study eye-opening
- 3 across my chin — to measure jaw clenching
The last sensor was to measure how much I snore. I had to make a snoring sound — so Sandy could feel on my throat where the electrode should be placed on me. All of these sensors were attached with the electrode-scooped glue and gauze pads.
 The next sleep test accessory was the nasal tubing, which included:
The next sleep test accessory was the nasal tubing, which included:
- Tubing near each nostril with the tubing wrapped around each ear — to hold it in place (blue in picture)
- A nasal monitor hooked onto the tubing — to measure breathing in and out (white in picture)
NOTE: The small white loop under my nose is a part of that monitor, and it also holds the small white tube that is supposed to hang down and gently sit on my lower lip, to monitor breaths in and out of my mouth. (Sandy had a challenging time with that small piece. Evidently, it was too long and not curling correctly. She spent quite a bit of time all night adjusting that and cutting it shorter every time she came into the room.) - The pulse oximeter was placed on my right pointer finger — to measure oxygen levels in my blood
I was now completely wired and ready for action! Er, I mean sleep.
After one last trip to the bathroom (where I learned how to carry my data box like the world’s worst necklace around my neck and was careful to not let anything fall into the toilet or sink), I was then off to bed.
Measuring Sleep Apnea Episodes
While I was having all of my sleep test sensors connected, Sandy told me a few things about how the night would go:
- When I first got into bed, they would turn on and test the video & audio monitoring equipment.
- I would be given several commands to make sure all the sensors were still connected and working properly — commands like yawn, cough, snore, flex your feet, take a big deep breath in, squeeze your eyes, etc.
- Sandy said I needed to try to sleep on my back as much as possible, on my sides would be okay, but not on my stomach. Too bad for me as I’m a stomach sleeper — but I would try my best.
- I would need to sleep for a certain number of hours for them to obtain an adequate amount of information, including the number of “apnea episodes” if I had any.
Anatomy of a sleep apnea episode: As air flow stops during a sleep apnea episode, the oxygen level in your blood drops. Your brain responds by briefly disturbing your sleep enough to kick start breathing — which often resumes with a gasp or a choking sound. If you have obstructive sleep apnea, you probably won’t remember these awakenings. Most of the time, you’ll stir just enough to tighten your throat muscles and open your windpipe. In central sleep apnea, you may be conscious of your awakenings. Source
- Based on a complicated math and science formula, they would determine if I had a sufficient number of episodes to “qualify” and warrant the use of the CPAP machine. If that happened, Sandy would come into my room, wake me up, and put on my CPAP mask. I would finish the night sleeping with it — while they continued to monitor and take measurements. They would adjust the pressure of the air flow into the mask throughout the night to see which pressure would reduce the apnea episodes for me the best.
- Either way (whether I needed the CPAP machine or not), she would wake me up around 6:00 AM, and that would be the end of the sleep test.
Let The Sleep Study Begin!
So, we completed all of the monitoring tests, and I was finally ready to go to sleep.
Had I known how much was involved with the preparation, I would have asked for an earlier bedtime. Now it was nearly midnight, and I had to sleep for a certain number of hours in order to qualify for the CPAP. I was not eager to actually wear the mask — but while I was here I wanted to get as much out of the study as possible.
I wriggled around in the bed trying to find the most comfortable position with all of my new electrode connections. It actually was not as bad as I had expected. The 2 most awkward electrodes were the ones right on the bones behind each ear (especially the left one) which was kind of painful. I figured that was just the way it was supposed to feel — so I tried to ignore it.
For the next several hours, I tried to sleep. On my back. On one side, and then the other. Sandy asked through the audio speaker if I needed anything. I said “No” and continued laying there. I was tired, but my mind was racing and I just could not relax. I tried counting sheep, thinking happy thoughts, singing songs (in my head), praying – you name it, I tried it.
Finally, I decided to get up and go to the bathroom — so I hesitantly said, “Hello?” Sandy immediately answered and I asked for help. She came right in and unhooked all my stuff and put the necklace box around my neck. I told her about the painful electrode behind my ear, and she loosened and then reattached that cord — which helped.
Another couple hours of the same thing, and I got up for the bathroom again. That time I jokingly said to Sandy, “I think I might have slept for a minute there!” She said “Yeah, but just a minute or two.” I asked if I was the only one having trouble sleeping, and she said that everyone was having trouble tonight. But I was the only one who “needed to qualify” (for the CPAP mask).
Then she said, “I hope they don’t make you come back” – which really made my head spin. I had not considered that! If I didn’t qualify tonight, I would have to do all of this again! That really put a new fear into my head, and sleeping was once again out of the question.
I dozed, but did not really sleep all the way until my 6:00 AM wake-up call.
End Of The Test + My Sleep Study Results
Sandy came in and began the process of removing all my cords and electrodes. It was a very quick process — and after very short paperwork, I was ready to go.
Oh, wait – except for those huge globs of glue in my hair. Sandy said I was able to use the shower in my bathroom before I left, but all I wanted to do was get home and go to bed! I put some paper towels in my hat so glue wouldn’t get all over it, grabbed my pillow, and headed for home. It took several HOT washes to get all of the glue out of my hair. The statement “This will easily wash out in the morning” was highly exaggerated.
A week later, I met with my doctor to learn the results of my sleep study. I was expecting to hear something along the lines of “inconclusive results, must repeat test.”
Here’s what I actually heard about my sleep test results:
- I slept for 219 minutes.
- I did not achieve REM sleep at all.
- My heart and brain activity were normal — nothing out of the ordinary.
- My breathing was very shallow.
- I did not snore.
- Number of sleep apnea episodes = 5.
Even with such limited sleep time to work with, they conclusively determined that I do not have sleep apnea. WHEW!!! I was seriously relieved that I would not have to repeat the test or wear the CPAP mask. We’re still not sure why I don’t feel rested upon waking — but it appears that apnea is not the reason.
For obstructive sleep apnea sufferers, the Apnea-Hypopnea Index (AHI) and Respiratory Disturbance Index (RDI) are very important sleep study result measurements. An apnea incident is defined as any complete or nearly complete restriction of airflow that lasts for at least 10 seconds. Hypopnea indicates a 50% reduction in airflow that lasts for at least 10 seconds. Both apnea and hypopnea incidents must be combined with arousals and/or a 3% or greater reduction of the oxygen levels in your blood. If your sleep study results indicate an AHI score of 5 or greater i.e. if apnea or hypopnea incidents occur 5-15 times per hour, this is interpreted as mild sleep apnea, 15-30 indicates moderate sleep apnea and an AHI score over 30 is interpreted as severe sleep apnea . RDI is a broader measure of events that disrupt us during sleep including non respiratory events such as sudden leg movements. An RDI score of 20 or greater indicates sleep apnea. Source
Before You Participate In A Sleep Study…
Here’s what I learned after my first sleep study – and some things I wish I would’ve done differently:
 I had on my comfortable pajamas, but I wished I had my slippers too. Next time, I would take my slippers, and my own blanket.
I had on my comfortable pajamas, but I wished I had my slippers too. Next time, I would take my slippers, and my own blanket.- I wish I would have asked questions ahead of time — or done more Internet research. I do believe some of my anxiety and inability to sleep was due to processing all I had learned that night. I was very anxious about wearing the masks and the possibility of having to do a 2nd sleep study.
- I wish I would have done everything possible to replicate my own sleeping habits. Three things come to mind on this:
1) The room temperature was too cold. Sandy kept turning the air conditioning up, saying that I would be warmer than usual with all the equipment on. As the night went on, I knew I was too cold — but I didn’t say anything and that was a mistake.
2) When I get into bed, I turn my TV onto a channel with an old sitcom. I turn the volume way down and set the sleep timer for 20 minutes. Most nights I’m asleep before the TV shuts off. I don’t know if I would have been allowed to do that in the Sleep Center, but I should have asked. I honestly think it helps clear my head and helps me “shut down” for the night. I was unusually stressed with all the new thoughts running around my head, and it may have helped.
3) Ok, this one will sound strange. I would have told Sandy that while I am trying to sleep, listening to the low sound of a familiar sitcom, I usually find myself wriggling my toes. Not squeezing them tightly, just gently and perhaps methodically wriggling them. But during my sleep test, I very consciously thought about not wriggling them. I knew there were electrodes on my calves, checking for restless leg syndrome. I’m pretty sure they would be able to tell the difference between my “fall asleep wriggling” and restless leg syndrome — but I would at least have the conversation.
- While I was talking with my sleep tech Sandy, she asked who my sleep doctor was. Huh? Sleep doctor? I now know that I could have/should have been referred to a sleep specialist. My doctor admitted that she was not familiar with much of the information shared on my sleep study results. I wonder if there might be helpful information in it, and plan to consult a sleep doctor soon.
- Sandy also mentioned that some patients need to take medication in order to sleep enough during the sleep test. I wish I would have explored that possibility and discussed having that option ready — in case it was needed.
- I wouldn’t worry so much about wearing a sleep mask. Many people have adjusted quite well to wearing one and their sleep has been much improved. There are many helpful videos and articles on how to learn to live with a CPAP mask and machine.
I wish you the best of luck if you are scheduled for your own sleep study test. Read as much as you can, ask all your questions, and – most of all – relax! After all, it’s just sleep.
Helpful Info About Sleep Apnea & Sleep Studies
In addition to the links I’ve included above, here are some other resources to help you with your own sleep problems and potential sleep test:
- Video: What A Sleep Test Is Like
- Sleep Apnea Aids & At-Home Tests
- Can’t Fall Asleep? Try This
- Sleep Study Photos
- Treatment Of Sleep Apnea
- Sleep Apnea Pillow
I’ve been crafting for many years. I started with cross-stitching, then moved on to wearable art, projects with painted wood, fabric crafts, and paper crafts — which has transformed primarily into card making. I also do some rubber stamping and scrapbooking, but mostly I enjoy creating handmade, one-of-a-kind cards.