It was 8:15 AM on a Wednesday morning.
It was 8:15 AM on a Wednesday morning.
The phone rang and I’m thinking, “I wonder who is calling so early.”
I hear Jim responding to the caller:
“Yes. Hi. Okay. Sure. Um… I could be there in a few minutes.”
Then he hung up and said, “Well, that can’t be good. It was the dermatologist. They said they want to discuss my treatment options.”
Woah!
So that’s how we found out Jim has skin cancer.
Once we arrived at the dermatologist’s office, we learned that it’s not just skin cancer… it’s melanoma skin cancer.
While melanoma is the least common type of skin cancer, it is by far the most virulent. It is the most common form of cancer among young adults age 25 to 29. Melanocytes are cells found in the bottom layer of the epidermis. These cells produce melanin, the substance responsible for skin pigmentation. That’s why melanomas often present as dark brown or black spots on the skin. Melanomas spread rapidly to internal organs and the lymph system, making them quite dangerous. Early detection is critical for curing this skin cancer. Source
There Was This One Mole…
Twenty days earlier, Jim had gone to the dermatologist to have a mole on his arm looked at.
It was a spot that we had casually watched over the past 6 years change from a regular brown mole, to a darker brown mole, to a lighter brown mole surrounded by very pink skin after being in the sun for a long time, to clear in the center and brown around the edges.
While I was a little bit concerned and asked Jim to have it looked at, he wasn’t at all concerned with this spot on his arm.
Here are some of Jim’s earliest skin cancer photos featuring the mole in question (before we knew it was cancer):





Hindsight is always 20/20. Now, looking back at the pictures, it’s pretty clear that Jim’s mole did follow the A-B-C-D-E guide which is commonly used to identify melanoma skin cancer.
It’s just that over the course of those 6 long years, there was never a dramatic change or a super obvious clue that made us think, “Oh yeah, that mole looks bad!”
People didn’t think twice when they saw that mole on his arm. Even our primary care physician said, “It’s probably nothing.”
What It’s Like To Have A Mole Biopsied
As a favor to me, when the mole changed from solid brown to clear in the center and brown on the edges, Jim went to the dermatologist to have it looked at.
They ended up cutting out the mole and having it biopsied. It was the standard routine for suspicious moles. The process is called a punch skin biopsy. (By the way, I wasn’t there, so I don’t have a biopsy picture — but Jim said his skin cancer biopsy was very quick, completely painless, and not as gruesome as that video makes it appear.)
On that day, the dermatologist told Jim, “It’s probably not anything serious, but we’ll biopsy it just in case.”
He came home that day with a rather deep gouge in his arm where the mole used to be, along with 3 stitches that had to be removed 10 days later.
The dermatologist assured us that the minor scar that he has now (next photo) from that very simple top-layer removal of the mole is nothing compared to what his arm is going to look like after the surgeon goes back in to that same spot to remove all traces of cancer that may have been surrounding the mole. He was very clear that after surgery, Jim’s arm will have a really huge scar — it might look as if a dog has taken a bite out of his arm!
TIP: If you even remotely think you have a mole that looks weird, have it looked at! And if your everyday doctor or primary care physician says, “It’s probably nothing” (as Jim’s did — approximately 5 years ago), you should still have it tested by a dermatologist just for the peace of mind. The earlier the better. And the smaller it is, the less of a scar you will have if it ultimately turns out to be malignant.
So the stains from Jim’s initial mole biopsy were reviewed by 2 separate pathologists to ensure that they were making the correct diagnosis of melanoma skin cancer. On a scale of 0 to 5 millimeters (in terms of depth of the melanoma tumor underneath the skin), Jim’s is 2.2 mm — a 5 is really scary, a 2.2 is in the “moderate” range.
According to the dermatologist, the severity of melanoma skin cancer is not based on how big it is on the skin, it’s based on how deep it goes in the skin:
- Up to 1 mm in depth, the only melanoma treatment required is regular skin checks (every 3 months) for 1 year.
- Over 1 mm in depth, the lymph nodes should be biopsied in order to determine if the cancer has spread and a large margin of the skin and tissue around the malignant site should be removed in order to assure that all of the cancer has been removed. (This is what Jim had to have done.)
Did You Know?…
Men have a higher overall incidence rate of melanoma skin cancer, thicker melanomas, and consequently, poorer outcomes than women. Source
Jim’s dermatologist was very clear: “It’s not a death sentence. However, this can be life-threatening. You have to treat this!”
Treatment For Melanoma Skin Cancer
 Since melanoma cancers can be life-threatening, the doctors don’t take any chances.
Since melanoma cancers can be life-threatening, the doctors don’t take any chances.
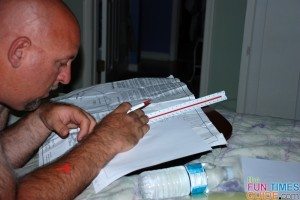
Jim’s first melanoma treatment was described to us like this:
- A surgeon will go back into the spot where the mole was and remove every possible trace of the cancer from that area. This means removing the melanoma tumor and about 3/4 of an inch of skin all around it.
- A sentinel node biopsy will be performed — where a radioactive substance will be injected near the tumor to locate the position of the sentinel lymph node (aka the first lymph node to which cancer cells are most likely to spread from the tumor).
- The surgeon will use a device that detects radioactivity to find the sentinel node. Then, he will make a small incision (about 1/2 inch) into the skin and remove that lymph node.
- The sentinel node will then be checked for the presence of cancer cells by a pathologist.
After having your lymph nodes checked, there are 2 possible melanoma treatment options:
- If there is no sign of cancer in the lymph nodes (which you will learn 7 to 14 days later), then you simply get skin checks (done by your dermatologist) every 3 months for the next 3 years — followed by skin checks every 6 months for the next 2 years. After 5 years, you’re considered cured, and your risk goes back to the normal population, similar to a person who’s never had skin cancer. In addition, your surgeon will want to conduct his own follow-ups by scheduling appointments at 6 months and 1 year after your surgery. He will do a complete head-to-toe physical (to check the skin and lymph nodes) and take a chest x-ray each time.
- If there is any trace of cancer in the lymph nodes, then more aggressive treatment options will be explored.
Here’s the best melanoma treatment info I’ve found online.
Melanoma Recurrence Rates
One stat that sticks with me is something I heard in a melanoma survivor’s story:
If the cancer has spread to the lymph nodes and they are able to remove all of it, then there’s a 65% chance the cancer will return within 5 years. (paraphrased)
I’ve since learned that number varies — depending on the depth of the tumor.
Jim’s melanoma tumor was 2.2 mm — he was given the following melanoma recurrence rates:
- Generally, for every millimeter of thickness, there’s a 10% risk that there will be cancer in the lymph nodes. In Jim’s case, his was 2.2 millimeters deep — so he had a 22% chance of having cancer in the lymph nodes.
- If they find no cancer in Jim’s lymph nodes, he will be considered Stage IIA, and there’s an 80% chance that he’ll never have cancer again. (Or a 20% chance that melanoma cancer will appear somewhere else in his body within 5 years.)
- If they do find cancer in Jim’s lymph nodes, they will probably take more lymph nodes just to be safe, and he will have a 40% chance that within 5 years melanoma cancer will pop back up somewhere else in his body. Chemotherapy is not an option — it just doesn’t work with melanoma cancer. There is an immune boosting therapy (a medication called Interferon) which reduces the chances of the cancer coming back, but only in 5% of the cases.
Here’s the best explanation of melanoma stages I could find.
Another thing that sticks with me is something that Jim’s dermatologist said: “After you experience what you’re going to experience, you’re never going to want to experience this again. So no tanning beds, and always wear sunscreen outdoors!” Jim’s surgeon later added, “That arm should stay out of the sun for a year — and always wear 30 SPF or greater on all other exposed areas, reapplying every hour.” (As the wife of someone with melanoma skin cancer, I immediately stopped using tanning beds and I started applying sunscreen more often.)
Treatment success depends on many factors, including the patient’s general health and whether the cancer has spread to the lymph nodes or other organs. If caught early, some melanomas can be cured. Deeper tumors are more likely to come back. If the skin cancer is deeper than 4 mm or the lymph nodes have cancer, there is a high risk of the cancer spreading to other tissues and organs. If the cancer has spread to the lymph nodes, there is a greater chance that the melanoma will come back. For patients with melanoma that has spread beyond the skin and nearby lymph nodes to other organs, treatment is more difficult. At this point, melanoma is usually not curable. Source
What Skin Cancer Looks Like
 Here are 38 pictures of skin cancers.
Here are 38 pictures of skin cancers.
Skin cancers are formed when new cells grow when they should not and old or damaged cells do not die when they should. These extra cells can form a mass of tissue called a growth (tumor). Source
As you can see, there are so many variations, it’s hard to tell which ones are melanoma skin cancer — which is why it’s important to just get a skin check once a year or so.
And if you have a mole that you’re unsure about… go with your gut and just get it checked!
- Here are photos showing what melanoma skin cancer looks like.
- Here are photos showing what basal cell carcinoma looks like.
- Here are photos showing what squamous cell carcinoma looks like.
Jim’s mole never really turned dark black like you typically see in photos of melanoma cancer. This has been slightly surprising to most of the doctors and nurses we’ve spoken with. When it was visible, it was usually a dark brown, but sometimes it faded to pink with brown around the edges — like it was when he had it biopsied.
While we first noticed that mole about 6 years ago, it seemed to come and go and it changed in appearance a lot over the years. It even looked like it was going away sometimes. In addition to the photos above, I have several more relatively close photos of his right arm taken during the same 6-year period where that mole is hardly noticeable at all.
Still, I wish Jim would have done something about this mole much earlier. Unfortunately, it never stood out to Jim as anything serious, so he didn’t want to “waste time” having it checked.
If only we knew then what we know now…
Non-melanoma cancer accounts for about half of all cases. It starts at basal cells or squamous cells, which are located at the base of the outer layer of skin or they cover the body’s internal and external surfaces. This type of cancer usually occurs on the sun-exposed areas of the body and it can spread quickly or slowly depending on its type. Fortunately, non-melanoma cancers rarely spread to other parts of the body. They are highly treatable and even curable if detected early. Melanoma is less common but the most dangerous. In 2010, 8,700 of the 11,790 skin cancer deaths resulted from melanoma. It starts in the melanocytes, the cells that produce skin pigment. Because of its relationship with skin color, individuals with fair skin are at a higher risk. Additionally, people with abnormal moles, a large number of moles, and people with a history of severe sunburns are more likely to develop melanoma. Source
And further…
Melanomas look like moles and often do grow inside existing moles. That’s why it is important for people to conduct regular self-examinations of their skin in order to detect any potential skin cancer early, when it is treatable. Most melanomas are caused by overexposure to the sun beginning in childhood. This cancer also runs in families. Source
Here’s how to do a head-to-toe check for skin cancer. Use this body map to keep track of your moles and freckles and their size, shape, and color over time. (Take it to your dermatologist and ask them to add their own notes & findings to your body map.)
More About Melanoma Skin Cancer
In addition to the melanoma treatment and diagnosis links I’ve included above, here are some other resources to help you understand melanoma skin cancer better:
- A Melanoma Skin Cancer Survivor Story (part 2 here)
- Facts & Stats About Melanoma Skin Cancer
- What Recurrent Malignant Melanoma Looks Like
- Photo Of Melanoma Skin Cancer On The Face
The next step: See Jim’s melanoma cancer surgery & recovery photos